
Deductible, Coinsurrance, Copay are they trying to speak English?
First let’s break it down for an elementary lesson in insurance. If you have little understanding of what deductible, coinsurance, and copay mean, you are in the majority of people we work with (Including many therapists!) So don’t feel bad! Insurance lingo is unfortunately overcomplicated sometimes and there aren’t often helpers available to educate us on what our policies actually mean. Shouldn’t we understand what we are buying?! So here goes…
Deductibles: This is the large scary number that we fear on our policies and understand to be the massive amount we will owe before insurance will pay for our services. Basically, this amount has to be paid before insurance will pay their share. It can be paid down bit by bit if you seek smaller services like counseling appointments, or all at once if you seek a more expensive service like a hospital stay.
I better Wait until my deductible is met…
For just a moment, I’d like to speak to those of you with a deductible that you find too daunting to seek services you need. So many times we hear people wanting to access services, but they hold off to “wait until their deductible is met”—this is a backwards notion that is based on our illogical fear of the deductible. The deductible isn’t a magic account that fills at a certain date after which you can get all the services you need. You pay it. Whether you pay it now or later just depends on the services you need. If anything—if you anticipate using a lot of services (doctors, procedures, therapy, etc) throughout the year, it makes more sense to start early in the year because then you are more likely to have necessary services get covered outside of what you pay.
Special note: some insurance plans are less straightforward than others—shame on them! They may have separate deductibles for separate types of service. If you think this could apply to your plan be sure to ask what services are “subject to the deductible”.
Copay: A copay is a set amount that you are responsible to pay before your insurance will cover their part. This is usually collected up front at the clinic. This does not get you any credit towards meeting your deductible, it’s just something you can expect to pay each time you seek a particular service. This amount might be different for different services too, so you could have a different copay amount for a doctor and a specialist and a therapist.
Coinsurrance: This is very similar to the copay except it is a percentage of the cost of the service rather than a flat rate. These do not usually contribute to the deductible total either, and usually they become active after the deductible is met. These are not typically paid up front, because they have to be calculated based on the contracted rate which providers don’t always know prior to billing.
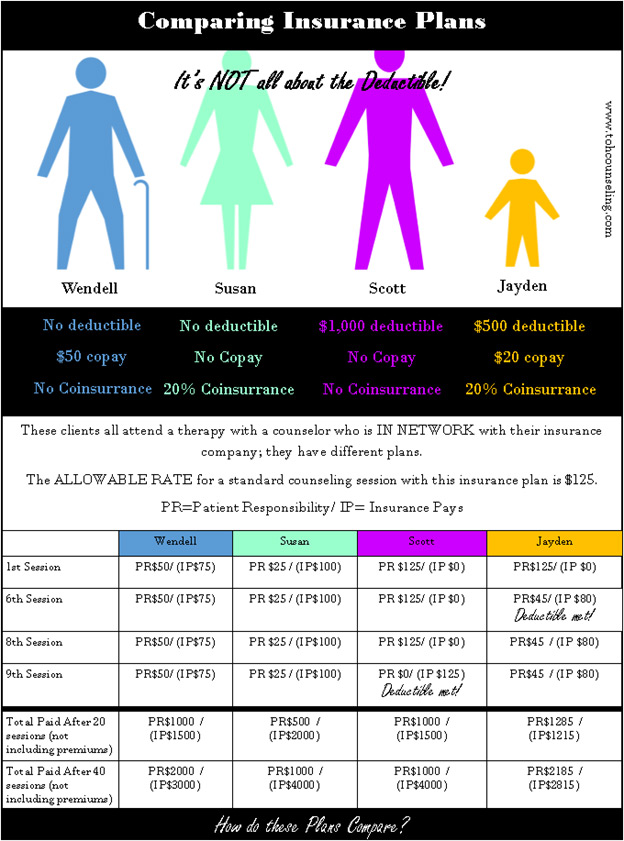
Contracted Rate/ Allowable Rate: This is the amount your insurance company determines they are willing to pay for a particular service. If your therapist is in network, they have agreed to accept this rate as payment in full for the service (meaning you receive a substantial discount on services based on the therapist’s agreement with your insurance company.)
In/ Out of Network: If your therapist is out of network, that means they have not agreed to accept this rate as payment in full. If you see an out of network provider, you will likely be responsible for their full rate, but if you have out-of-network coverage, your insurance might reimburse you for a portion of the service (up to the insurance’s allowable rate).
Prior Authorizations: Some plans require getting special permission in order to seek certain services. If this is required, you may have to ask your therapist to complete these processes on your behalf.

Service Limits: Some plans limit the number of services you can receive within a calendar year. This DOES NOT mean that it will be impossible to receive further services; however, your therapist may have to go through an additional authorization process to prove medical necessity for further sessions.
Medical Necessity: This term is a best practice ethical guideline for all medical professionals meaning that we only provide services to the extent that a client needs them. Your mental health professional is the determiner of your medical necessity—NOT your insurance, even though they sometimes try to share their input to limit services.
Diagnosis: This is the clinical label that is used to describe the issues/ concerns bringing you to counseling; it is a part of demonstrating medical necessity. You may have heard that insurance cannot be billed without your therapist ascribing you a diagnosis—and this is correct. Not all diagnoses carry the same stigma or weight clinically and some diagnoses are temporary, but allow you to receive the services you need. Not all therapists discuss every diagnosis with their clients, but if you have concerns about this, you should discuss them with your therapist. If you have other questions about the information that your insurance receives as part of billing insurance, you can also ask your therapist.
What are the right questions I need to ask my insurance before I schedule an appointment?

- Is this therapist/ Clinic considered In Network with my Insurance Plan?
- (If considering an out of network provider) Does my plan offer out of network benefits for outpatient mental health services?
- Does my plan cover outpatient individual/ family (NOT “couples”)/ group counseling?
- What Patient Responsibility do I have on my plan for these services?
- Do I need any prior authorizations to seek these services?
You need to be your own advocate and remember your insurance is supposed to provide you with coverage to get the services you need. You always have the choice NOT to use your insurance to cover your services, and there are processed for you to file complaints if you feel you are not being treated right by your insurance. Don’t let your insurance dictate your mental health care.
January 2019, Jennifer Beall, MA, LPCC
